Not long after the first wave of COVID-19 infections, doctors around the world began to notice something strange – a series of persistent effects that persist in patients, long after they appear to have recovered from the virus.
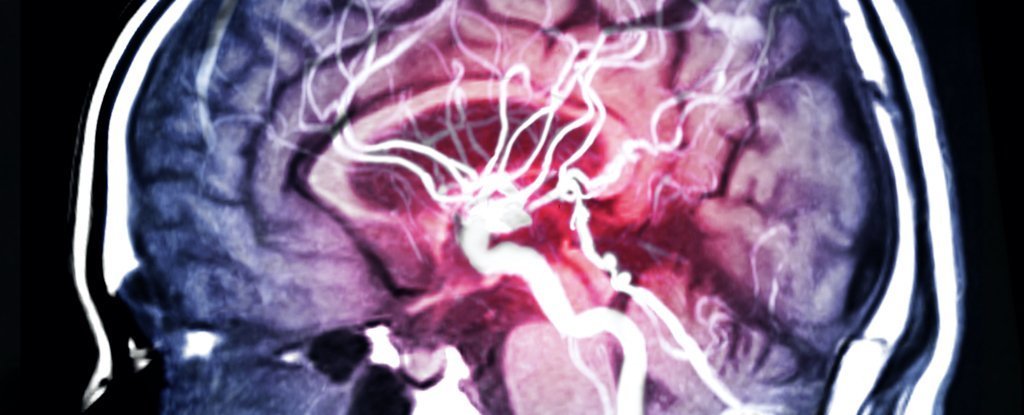
These unusual neurological symptoms – including fatigue, memory loss, confusion and other abnormalities – are sometimes known as ‘brain fog’ or ‘brain COVID’, and new research may have identified an underlying cause of the disease.
“We were initially approached by our intensive care colleagues who observed severe delirium in many patients hospitalized with COVID-19,” said neuro-oncologist Jessica Wilcox of the Memorial Sloan Kettering Cancer Center (MSK) in New York.
“This meeting turned into a tremendous collaboration between neurology, intensive care, microbiology and neuroradiology to learn what was going on and to see how we could better help our patients.”
As part of the new study, Wilcox and his fellow researchers examined the cerebrospinal fluid of 18 cancer patients who had neurological dysfunction (also known as encephalopathy) after being infected with the SARS-CoV-2 virus.
Initially, it was suspected that an ongoing viral infection could be the cause of his brain fog symptoms, but microbiological analysis of the fluid collected in lumbar punctures revealed no sign of the virus, suggesting that the patients had recovered from COVID-19 .
However, the research revealed an important clue as to what was going on.
“We found that these patients had persistent inflammation and high levels of cytokines in the cerebrospinal fluid, which explained the symptoms they were experiencing,” explains researcher MSK and co-author of the study, Jan Remsik.
Cytokines are a broad category of proteins involved in signaling the immune system.
In some cases of coronavirus, an overproduction of these molecules results in what is known as a cytokine storm, which can cause excessive inflammation and is potentially deadly.
A similar phenomenon showing high levels of inflammatory cytokines is sometimes seen as a side effect of chimeric antibody receptor (CAR) T cell therapy, an immunotherapy treatment, which can also produce confusion, delirium and other neurological effects that have a resemblance to the brain COVID fog.
The thought is that the flood of these inflammatory chemicals in the immune system infiltrates the brain, producing symptoms of encephalopathy as seen in patients.
Although this is the largest study to date to demonstrate this potential link between COVID-19 and the post-infection neurological effects, we will need much more data to uncover this association.
That said, the findings here suggest that anti-inflammatory drugs may be useful in mitigating brain fog in patients and may highlight new directions in terms of diagnosing this strange and persistent malaise.
“We used to think that the nervous system was an organ with immunological privileges, which means that it had nothing to do with the immune system,” explains neuro-oncologist Adrienne Boire of MSK.
“But the more we look, the more we find connections between the two.”
The results are reported in Cancer cell.