Artificial intelligence and machine learning systems continue to be adopted in an increasing range of health applications, such as assisting doctors in medical imaging diagnostics. Able to understand X-rays and generate MRIs quickly – sometimes even capable of detecting cases of COVID – these systems have also been shown to be effective in detecting early signs of breast cancer that might otherwise go unnoticed by radiologists . Google and IBM, as well as medical centers and university research teams around the world, have been looking to develop these cancer detection algorithms.
MIT
They can detect worrying lumps as well as radiologists and predict the future appearance of the disease “significantly” better than the humans who trained them. However, many medical AI imaging systems produce markedly less accurate results for black and brown people – although WOC is 43 percent more likely to die of breast cancer compared to its white counterparts.
“African American women continue to develop breast cancer at younger ages, and often at more advanced stages,” said Salewai Oseni, a breast surgeon at Massachusetts General Hospital, in a recent statement to the press. “This, together with the highest number of triple negative breast cancer cases in this group, has resulted in increased breast cancer mortality.”
Over the past two years, researchers from MIT CSAIL and the Abdul Latif Jameel Clinic for Machine Learning in Health have worked to develop a new deep learning system, capable of predicting a patient’s risk of cancer, taking advantage of only the person’s mammograms, which supposedly works with equal effectiveness regardless of race or ethnicity.
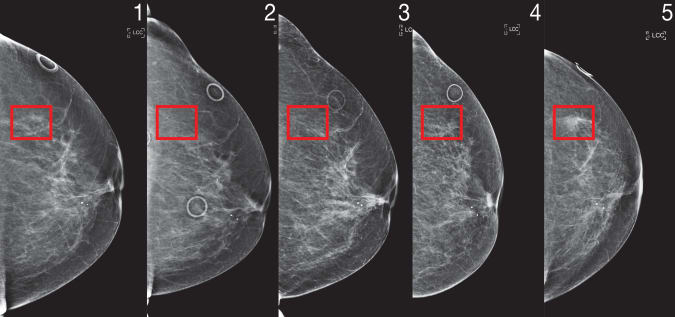
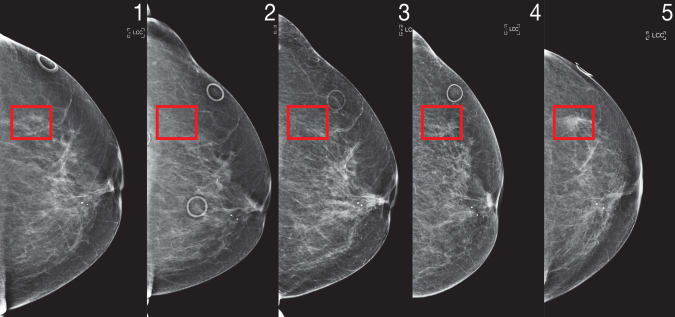
Called “Mirai” (not to be confused with Toyota’s fuel cell EV), this algorithm is supposed to be able to model “a patient’s risk at various future time points”, taking into account small variations, until the the clinic’s mammography brand uses, according to a statement Wednesday from MIT. Your predictions can be further optimized if other clinical risk factors – such as age or family history – are available.
The CSAIL team initially trained Mirai on a 200,000 exam data set from Massachusetts General Hospital (MGH) before validating their predictive results on additional sets from the Karolinska Institute in Sweden and the Chang Gung Memorial Hospital in Taiwan. So far, the results are highly encouraging with results suggesting that Mirai is “significantly more accurate,” according to the statement, in predicting cancer risks in patients in all three data groups and able to correctly identify almost twice as much potential cancer cases among high-risk groups. the Tyrer-Cuzick diagnostic model currently employed throughout the study.
To ensure that Mirai’s recommendations were consistent, the CSAIL team deviated the algorithm by running it through an adversary network to differentiate between aspects of mammography that are important and those caused by small random environmental variations (such as the / mammography machine model)
“Enhanced breast cancer risk models enable targeted screening strategies that achieve earlier detection and less damage to screening than existing guidelines,” Adam Yala, lead author of CSAIL Science, Translational Medicine study, said in a statement. “Our goal is to make these advances part of the standard of care.”
MIT
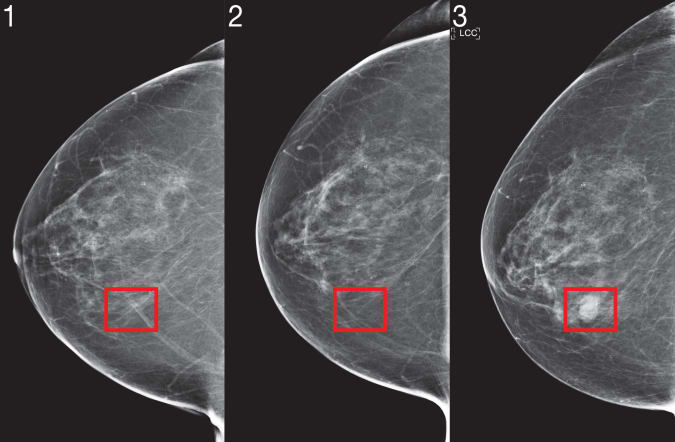
This could advance the state of cancer science. Modern mammograms still have reliability problems, even now 60 years after the widespread adoption of the technology. Experts still disagree on how often women should be screened, some arguing for more aggressive strategies to detect cancerous tumors as early as possible, while others advocate longer intervals between routine tests in order to minimize rates false positives (as well as maintaining reduced medical costs for patients). Mirai will be used to help doctors determine which patients would benefit most (and most equitably) from undergoing complementary imaging and MRI scans based on the mammogram image and other factors such as a person’s age, genetics, family medical history and density of breast tissue.
“We know that MRI can detect cancer before mammography and that early detection improves patient outcomes,” explained Yala. “But for patients at low risk for cancer, the risk of false positives may outweigh the benefits. With improved risk models, we can design more differentiated risk screening guidelines that offer more sensitive screening, such as MRI, for patients who will develop cancer, for better results while reducing unnecessary screening and overtreatment for the rest. “
Mirai also takes into account risk factors that do not necessarily appear on mammography, such as the patient’s age, hormone levels and menopausal status. These factors are ingrained during the training phase, allowing the model to predict them based on the mammography image provided, even if the doctor does not provide this information manually.
Moving forward, Mirai could find use in other medical applications for the benefit of the community. Although the system may not be able to interpret a patient’s existing imaging result history and integrate it into his assessment, it can be based on any additional X-rays / MRIs provided to him in the future. The team is also considering integrating tomosynthesis techniques to further increase Mirai’s statistical fitness. The CSAIL team also partnered with researchers at Emory University to further validate the model.