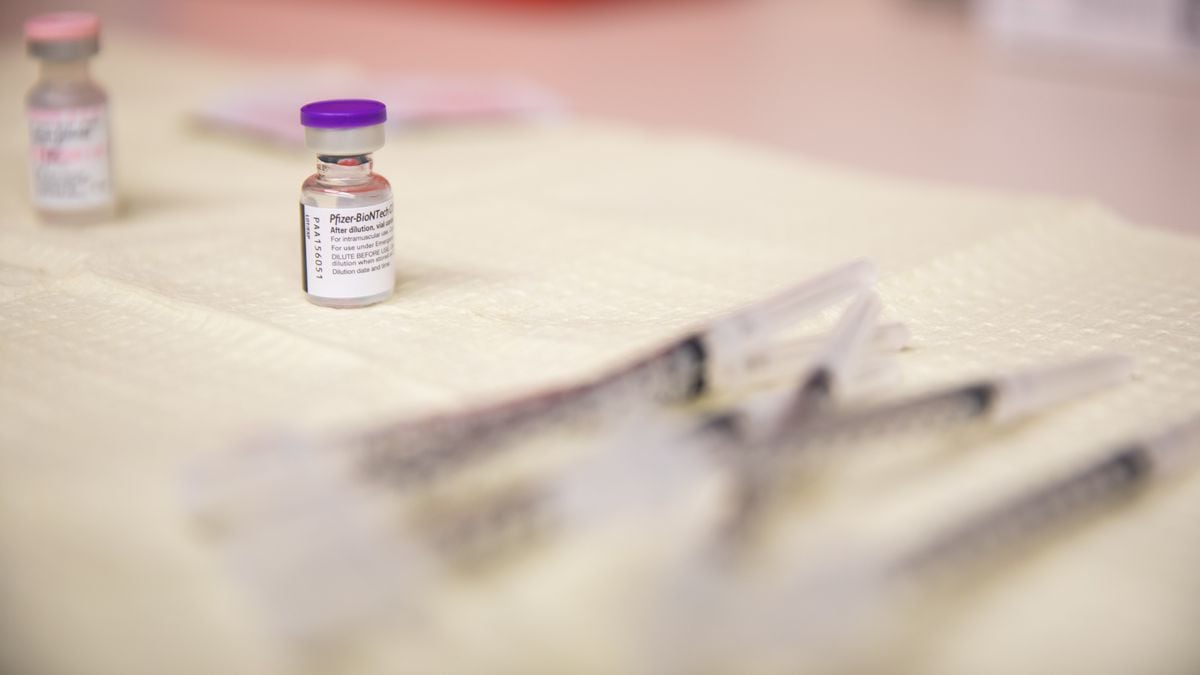
A closed vial of the Pfizer-BioNTech COVID-19 vaccine at Deschutes County Department of Public Health in Bend, Oregon, Tuesday, January 12, 2021.
Bradley W. Parks / OPB
This week, Kaiser Permanente launched a COVID-19 vaccination clinic at the Oregon Convention Center in partnership with three other major health systems: Providence, Legacy Health and OHSU.
It is the first mass vaccination site in the Portland area and a key step in the state’s effort to build a system that can eventually be expanded to inoculate more than 3 million adult Oregonians.
The convention center clinic will be by appointment only and will start vaccinating around 2,000 people a day. As more doses become available, Kaiser and its partners say the site should be able to vaccinate up to 7,500 people a day.
“We are defining this as a sustainable operation that we will manage until we no longer need it,” said Wendy Watson, director of operations at Kaiser Permanente Northwest. “Our ultimate goal is for it to be open 7 days a week, at extended hours.”
The new website is an example of how Oregon, after a slow start, is doing a better job of taking doses of the vaccine out of the freezer and putting them in people’s arms: last week, vaccinators repeatedly exceeded the governor’s goal Kate Brown of 12,000 doses administered daily.
But the pace of vaccination still needs to increase for Oregon to achieve collective immunity and stop the spread of the virus: just over 6% of the adult population has received at least one dose of the COVID-19 vaccine so far.
Getting there is complicated and requires more than just large spaces to administer our vaccines. Here’s what more experts say the state needs to increase distribution successfully:
More vaccines
Each week, Oregon is receiving approximately 100,000 vaccines in total, including the first and second doses of the Pfizer COVID-19 vaccine and the Modern COVID-19 vaccine. If that sounds like a lot, consider that there are about 3.3 million adults in Oregon, and each needs two doses.
It would take almost double the current supply to fully vaccinate all Oregon adults by the end of autumn.
Patrick Allen, director of the Oregon Health Authority, said the lack of supplies is the main obstacle the state faces.
“We are now in a place where we can administer virtually as much vaccine as the federal government can provide us with,” Allen said at a press conference for the convention center clinic.
Across the state, hospital systems and other partners have stepped up efforts to administer injections – and are now begging for more doses. But the supply from manufacturers remains limited.
“Until we see a new vaccine approved, or see production increase significantly, everyone in the state, including this operation at the convention center, will be able to vaccinate more people than we have vaccines,” said Allen.
In fact, approval of a new vaccine may soon help alleviate supplies shortages in Oregon and other states.
A third vaccine candidate, from Johnson & Johnson, is nearing the end of clinical trials. Depending on what the data shows, he may go to federal regulators for emergency approval in February.
An army of volunteers
Oregon needs more trained vaccinators and more staff to support them.
Before a person can be vaccinated, they may need help finding out where to park. They must sign a consent form and undergo screening for factors that can complicate vaccination. After receiving the injection, patients should be observed for 15 to 30 minutes in a clinical setting in case of an allergic reaction.
All of this requires additional volunteers.
Health systems are calling on retired nurses and doctors to help staff vaccination sites, so that their regular doctors can focus on treating patients with COVID-19 and everyone in need of care.
Another source of support: the Oregon Air National Guard and the Oregon Army National Guard.
Oregon has approximately 8,300 Army and Air guards. Several hundred have medical qualifications and can administer injections, but the guard’s primary role is likely to be to provide logistical support and non-medical volunteers to vaccination sites.
Vaccines at the pharmacy
Pharmacies are currently playing a key role in providing the vaccine to residents in long-term care and memory care, taking them directly to the facility.
And the state and the CDC have the potential to activate a much broader pharmacy partnership, which could deliver the vaccine directly to retail pharmacies across the state – potentially allowing eligible members of the public to be vaccinated at their local pharmacy for free.
The pharmacies participating in the federal program include many well-known names, including CVS, Walgreens, Fred Meyer and Costco.
The governor said earlier this month that the state expected shipments to pharmacies to arrive soon.
It is now unclear whether this happened or whether the federal government is sending Oregon enough vaccine to activate the pharmacy program. A week after Brown said the state was in the process of launching it, she and other governors accused Health and Human Services Secretary Alex Azar of promising more doses than the federal government could actually deliver.
The Oregon Health Authority has not responded to a request for an update on when retail pharmacies in Oregon will begin receiving the vaccine.
A plan for essential workers
COVID-19 did not impact all Oregon residents equally. Case rates are twice as high for black and Native American Oregonians as for whites. For Pacific Islanders and Latinos, the disparity is even greater: they are three times more likely to get COVID-19 than a white Oregonian.
National surveys have found that one of the main reasons for these disparities is that specific racial and ethnic communities are overrepresented in low-paid jobs that cannot be done remotely, and are more likely to be exposed to the virus at work.
“I would like to bring this to the forefront of the conversation,” said Daniel Lopez-Cevallos, professor of health equity and ethnic studies at Oregon State University. “We have essential workers out there, being exposed, day after day.”
Lopez says that, at the very least, the governor needs to make it clear when essential workers will be prioritized for vaccination. The state’s vaccine advisory committee has placed them in the broader group – IB – which will have priority some time after teachers and adults aged 65 and over, but before the general population.
Lopez-Cevallos would like to see the state planning a specific vaccination strategy for essential workers.
Melissa Unger, director of SEIU Local 530, shares Lopez-Celvallos’ concern: the state does not yet have a targeted plan to reach the essential workers who have been most affected by the virus.
Unger believes essential workers are at risk of falling behind if the state is too dependent on mass vaccination sites, because they won’t have time to wait in line or lurk online for new appointments.
“They have to go to work. We need to make sure that we are making this process work for the same people who were asked to keep our economy running during this pandemic, ”said Unger.
Unger’s suggestions include a dedicated scheduling line that allows essential employees to schedule their vaccines and better dissemination – through text and in people’s native languages.
More and better public health communication
Both Unger and Lopez say the state needs a more aggressive public health message campaign to reassure people and answer their questions about the vaccine.
Unger says that not all health professionals and hospitals currently eligible for the vaccine feel comfortable receiving it. They are a heterogeneous group that includes people with varying degrees of health education: certified nursing assistants, people who clean hospitals and provide food services and health assistants at home, for example.
Unger says many of them are trying to decide whether to get vaccinated and need more help getting answers to their questions.
“What are we doing as a community and state to make sure they have the answers they need to feel safe?” Unger said.
Unger also thinks the state needs to do a better job, assuring the public that there is a plan to bring the vaccine to everyone – it will take time.
“The scarcity element in a pandemic is very dangerous,” she said. “‘Everyone is trying to figure out how to feel safe and protected for their families now, and I think the role of the government is to be able to communicate that we are going to get there, and there is hope.”