Doctors say a woman in Michigan contracted Covid-19 and died last fall two months after receiving a contaminated double lung transplant from a donor who revealed she harbored the virus that causes the disease – despite showing no signs of illness and initially have a negative result.
Officials at the University of Michigan School of Medicine have suggested that this may be the first proven case of Covid-19 in the United States where the virus was transmitted through an organ transplant. A surgeon who treated the donor’s lungs was also infected with the virus and fell ill, but later recovered.
The incident appears to be isolated – the only confirmed case among almost 40,000 transplants in 2020. But it has led to more complete testing requests from lung transplant donors, with samples taken from inside the donor’s lungs, as well as from the nose and throat, said Dr. Daniel Kaul, director of the transplant medicine infectious disease service at Michigan Medicine.
All the screenings that we normally do and are able to do, we did.
“We would not have used the lungs at all if we had a positive Covid test,” said Kaul, who coauthored a report on the case in the American Journal of Transplantation.
The virus was transmitted when the lungs of an Upper Midwest woman, who died after suffering a severe brain injury in a car accident, were transplanted into a woman with chronic obstructive pulmonary disease at University Hospital in Ann Arbor. Nose and throat samples routinely collected from organ donors and recipients tested negative for SARS-CoV-2, the virus that causes Covid-19.
“All the projections that we normally do and are able to do, we did,” said Kaul.
Complete coverage of the coronavirus outbreak
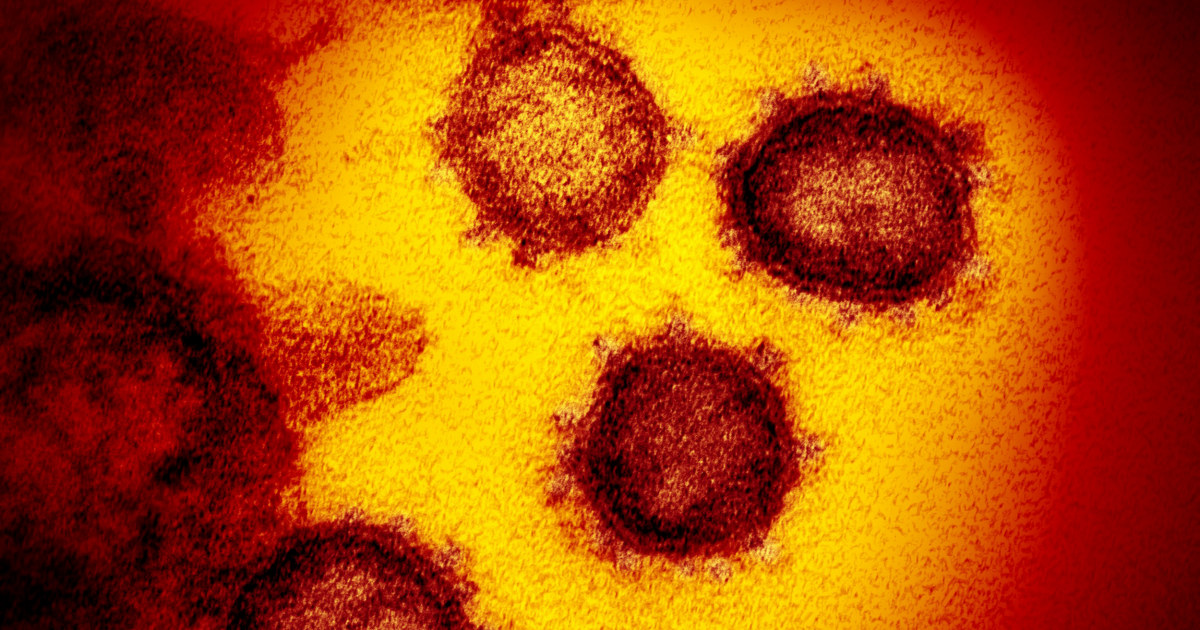
Three days after the operation, however, the recipient developed a fever; his blood pressure dropped and his breathing became difficult. The image showed signs of lung infection.
As her condition worsened, the patient developed septic shock and heart function problems. The doctors decided to take the SARS-CoV-2 test, said Kaul. The samples from his new lungs were positive.
‘A tragic case’
Suspecting the source of the infection, doctors returned to donor samples for transplantation. A molecular test of a donor nose and throat swab, done 48 hours after obtaining the lungs, was negative for SARS-Cov-2. The donor’s family told doctors that she had no history of recent travel or symptoms of Covid-19 and no known exposure to anyone with the disease.
But doctors kept a sample of the fluid washed out of the donor’s lungs. When they tested that fluid, it was positive for the virus. Four days after the transplant, the surgeon who manipulated the donor’s lungs and performed the surgery also showed a positive result. Genetic screening revealed that the transplant recipient and the surgeon were infected by the donor. Ten other members of the transplant team tested negative for the virus.
The transplant recipient deteriorated rapidly, developing multisystem organ failure. Doctors tried known treatments for Covid-19, including remdesivir, a newly approved drug, and convalescent blood plasma from people previously infected with the disease. Eventually, she was put on the option of last resort of ECMO, or oxygenation by extracorporeal membrane, without success. Life support was withdrawn and she died 61 days after the transplant.
Kaul called the incident “a tragic case”.
While the Michigan case marks the first confirmed incident in the United States of transmission through a transplant, others have been suspected. A recent report by the Center for Disease Control and Prevention analyzed eight possible cases of what is known as a donor-derived infection that occurred last spring, but concluded that the most likely source of transmission of the Covid-19 virus in these cases was in a community. or health center context.
Before that incident, it was not clear whether the virus could be transmitted through solid organ transplants, although it is well documented with other respiratory viruses. Transmission of the 2009 H1N1 flu pandemic by donors has been detected almost exclusively in lung transplant recipients, noted Kaul.
Large sample required
While it is not surprising that SARS-CoV-2 can be transmitted through infected lungs, it remains to be seen whether other organs affected by Covid-19 – heart, liver and kidneys, for example – can transmit the virus as well.
“It appears that for non-pulmonary donors it can be very difficult to transmit Covid, even if the donor has Covid,” said Kaul.
Organ donors were routinely tested for SARS-CoV-2 during the pandemic, although it is not required by the Organ Procurement and Transplantation Network, or OPTN, which oversees transplantation in the USA. But the Michigan case highlights the need for broader sampling before transplantation, especially in areas with high Covid-19 transmission rates, Kaul said.
When it comes to lungs, that means making sure to test samples from the donor’s lower respiratory tract, as well as the nose and throat. Obtaining and testing these donor samples can be difficult to do in a timely manner. There is also a risk of infection in the donated lungs, Kaul said.
Since no organ other than the lungs was used, the Michigan case does not provide information on the testing protocols for other organs.
Overall, viral transmissions from organ donors to recipients remain rare, occurring in less than 1 percent of transplant recipients, the research shows. The medical risks faced by sick patients who reject a donor organ are generally much greater, said Dr. David Klassen, medical director for the United Network for Organ Sharing, the federal contractor who administers the OPTN.
“The risks of refusing transplants are catastrophic,” he said. “I don’t think patients should be afraid of the transplantation process.”