A gene silencing technique based on CRISPR may relieve pain in mice, according to a study1. Although the therapy is still a long way from being used in humans, scientists say it is a promising approach to suppress chronic pain that lasts for months or years. Chronic pain is usually treated with opioids, such as morphine, which can lead to addiction.
“It is a real challenge that the best drugs we have to treat pain give us another disease,” says Margarita Calvo, pain doctor at the Pontifical Catholic University of Chile in Santiago, who was not involved in the research. That’s why the CRISPR-based technique is exciting, she says.
Scientists are already evaluating CRISPR therapies that edit a person’s genome as treatments for blood disorders and some forms of hereditary blindness. The new version of CRISPR does not directly edit genes – it prevents them from being expressed – and, therefore, should not cause permanent changes, although it is not clear how long their effects last.
A new way to manage pain
Some studies estimate that a large proportion of the population in Europe and the United States – up to 50% – experience chronic paintwo,3. This pain can become debilitating over time, limiting a person’s activity and having a negative effect on their mental health. Despite the prevalence of the disease, there are few options for providing long-term relief without side effects. Even so, doctors are moving away from opioid prescription due to the risk of addiction, which has further reduced their options.
This situation inspired bioengineer Ana Moreno and colleagues at the University of California, San Diego, to seek alternative treatment.
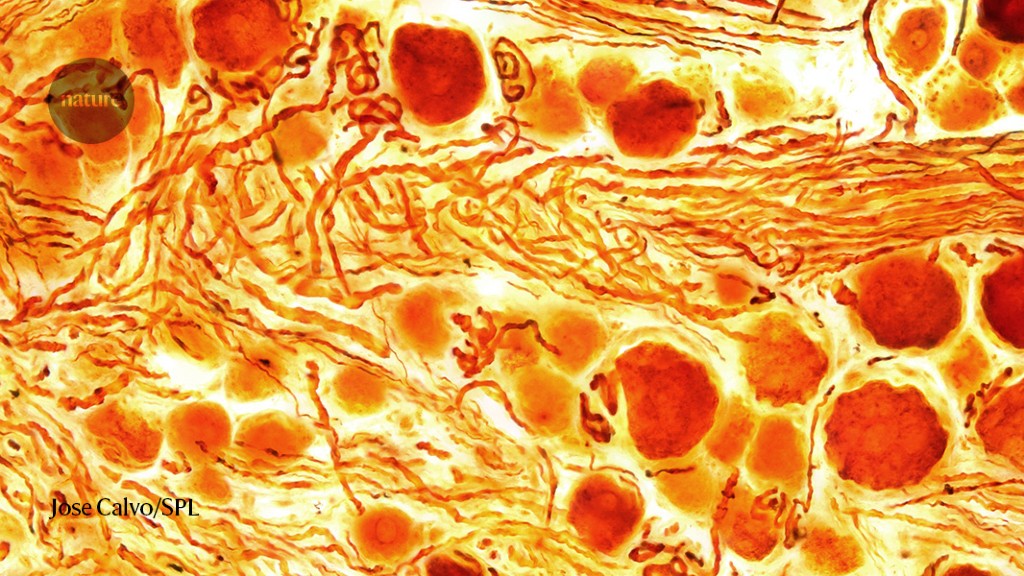
Pain is registered in the brain when a stimulus – such as touching a scorching pan or being poked with a sharp object – triggers neurons to send an electrical signal through the nerves of the spinal cord and upwards to the brain. This happens when pore-like openings along the neuron – called ion channels – open and close to allow the ions to pass, which transmits a current along the nerve. With chronic pain, parts of this pathway can become overactive.
Although there are many types of ion channels, studies have suggested that a sodium channel called Nav1.7 can play a central role in chronic pain. When people have mutations in the gene that encodes that channel, they experience extreme and constant pain or are unable to feel any pain at all.
So Moreno and his team thought they might be able to stop pain signals that travel to the brain, preventing neurons from producing Nav1.7. Chemists have been trying to block Nav1.7 with small molecule drugs and antibodies, but have struggled because these therapies also interact with structurally similar sodium channels in the body, causing side effects, including numbness and poor coordination. But with CRISPR, which targets genes accurately, researchers thought they might be able to target Nav1.7 directly, without any off-target effects.
Leveraging the accuracy of CRISPR
The team started with a modified version of the Cas9 protein that is normally part of the CRISPR gene editing system. It could target, but not cut, the DNA sequence that encodes Nav1.7. The researchers attached to the modified Cas9 a second “repressor” protein that disrupts Nav1.7 gene to be expressed. The researchers packaged this system into a small inactive virus called an adeno-associated virus, which could transport it into cells.
They gave the mice a spinal injection of gene silencing therapy, then tried to induce chronic pain by injecting the animals with chemotherapy drugs or inflammatory agents. These mice were more tolerant of painful stimuli. And mice that were already suffering from chronic pain benefited from the therapy, the team showed. For example, mice that received doses of chemotherapy became very sensitive to pain, but lost that sensitivity after a single injection of gene therapy. The results were published in Science, Translational Medicine on March 101.
Pain relief seemed to last, in some cases, up to 44 weeks after the injection. “This is remarkable,” says Sulayman Dib-Hajj, a neuroscientist at Yale University in New Haven, Connecticut.
It is important to point out, says Calvo, that the treatment seems to have lowered the expression of Nav1.7 without switching off other sodium channels – the rats did not lose any sensation other than pain and had no other side effects.
Despite the excitement, scientists warn that these results are still preliminary and do not know whether the pain relief seen in mice will translate into humans. “It gives us hope that gene therapy approaches can work in humans” to treat chronic pain, says Dib-Hajj, “but more work needs to be done.”
Moreno is now the chief executive of Navega Therapeutics in San Diego, which plans to continue developing the treatment with the hope of one day testing it in humans.