Since the new coronavirus, SARS-CoV-2, started to jump from human to human, it is mutating. The molecular machinery the virus uses to read and make copies of its genetic code is not good at review; minor typos made in the copy process may not be corrected. Each time the virus hits a new human victim, it infects a cell and makes an army of clones, some carrying genetic errors. These buggy clones continue, infecting more cells, more people. Each cycle, each infection offers more opportunities for errors. And, over time, these errors, these mutations, accumulate.
Some of these changes are meaningless. Some get lost in the frantic making of viruses. But some become permanent elements, passed from virus to virus, from human to human. Perhaps this happens by chance; maybe it’s because the change helps the virus to survive in some way. But together, viral strains that carry a notable mutation can start to carry others. Collections of notable mutations begin to emerge in viral strains and sometimes appear to have an advantage over their relatives. That’s when these distinct viruses – these variants – are concerned.
Scientists around the world have been watching mutations and variants closely since the beginning of the pandemic, watching some rise and fall without much effort. But in the past few months, they have been uneasy about at least three variants. These variants of concern, or VOCs, have raised critical questions – and alarms – about whether they can spread more easily than previous viral varieties, whether they can escape therapies and vaccines, or even whether they are more deadly.
Here, we’ll see what we know and what we don’t know about these variants. With a lot of research yet to be done, there are many unanswered questions. But researchers are working quickly to resolve the most important unknowns. At the top of the list is whether the vaccines we already have will be effective against the variants. So far, it seems likely. Even so, the virus is sending a clear message: with rampant transmission accelerating viral evolution, more variants will emerge and we need to be prepared.
With more data being made available each day, we will update this story with significant discoveries as they arise. Before getting to the data we have, a quick note about the names: it is problematic to identify diseases or infectious agents – in this case, virus variants – based on where they were identified. These geographical associations are at risk of creating stigma and may discourage reporting, so there is an active discussion in the scientific community about the best way to name current variants. In the meantime, it has become very common to refer to them by their country of origin. We will try to avoid this as much as possible, making it clear which variants we are talking about.
B.1.1.7
Alternative names: 501Y.V1 and VOC 202012/01
Geographical association: UK
Number of countries reporting cases: 70
Increased transmissibility: Yes
Increased disease severity / mortality: A “realistic possibility”
Vaccine effectiveness: Still effective
In early December 2020, researchers and UK officials began to warn of a new variant that appeared to be spreading abnormally quickly while carrying an unusually large number of mutations – 23. The first record of the variant in the UK dates back to two samples taken from infected people on 20 and 21 September. In a matter of weeks, the variant started to represent an increasing proportion of the total cases there. The researchers quickly suspected that the variant had evolved to become more transmissible – that is, it is able to spread more easily from person to person.
Streaming
Data analysis since December has supported this hypothesis, but researchers are still discovering just how much it is more transmissible compared to previous versions. In early January, UK researchers released preliminary results from a series of models that estimated variant adhesions at an additional 0.36 to 0.68 in the observed reproduction number of SARS-CoV-2. This means that, on average, people infected with B.1.1.7 will continue to infect a additional 0.36 to 0.68 people plus how many would have infected had they had an earlier version of the virus. More recent estimates have been approximately in this range, suggesting that B.1.1.7 has about 47% or 56% increase in transmission.
B.1.1.7 has now been detected in more than 60 countries in addition to the United Kingdom, including the United States, where it has been found in at least two dozen states. A modeling study published by the United States Centers for Disease Control and Prevention on January 15 estimated that it will become the predominant strain in the United States in March.
Mutations
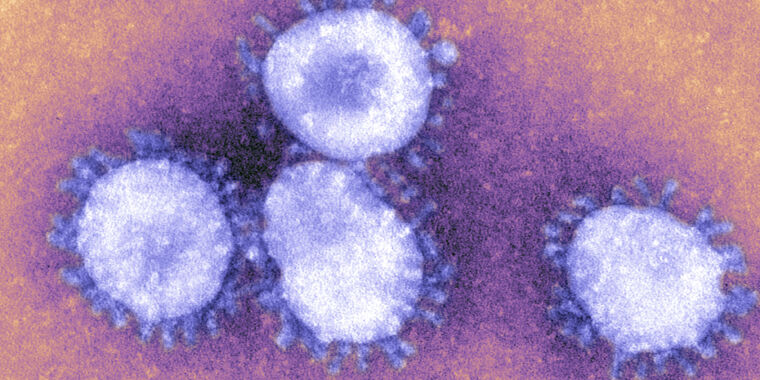
Some of the mutations that B.1.1.7 carry seem to help explain the virus’ newfound ability. The variant carries 23 mutations in all: 13 mutations that alter the virus protein sequences (not synonymous), four deletions and six synonymous mutations. Of the B.1.1.7 mutations, eight occur in the virus’s spike protein, the now notorious taco-like protein that protrudes from the virus’s spherical particle. Spike is what the virus uses to cling to and infect cells, which the protein does when it binds to a receptor outside human cells called ACE2.
So far, we know that at least three of the eight peak mutations in B.1.1.7 may be relevant to the driven transmission of the variant. The main one is a mutation that changes one of the critical amino acids in the peak proteins – the amino acid at position 501 of the peak protein sequence. Specifically, the mutation changes the amino acid at 501 from an asparagine (N) to a tyrosine (Y), so the mutation is written as N501Y. The 501 amino acid is critical because it is within the peak area that binds directly to ACE2 – called the receptor binding domain (RBD) – and is one of only six key contact residues in the RBD. Laboratory experiments suggested that changing from an N to a Y in 501 increases the peak’s ability to bind to ACE2, and experiments in mice have linked the mutation to increased infectivity and disease.
After N501Y, there is P681H. The mutation at position 681 – changing the proline amino acid (P) to histidine (H) – falls close to a single furin cleavage site in the SARS-CoV-2 spike protein. For SARS-CoV-2 to successfully enter a cell after binding to ACE2, the spike protein needs to be cleaved into its two subunits by enzymes. The division changes the conformation of the peak and activates it, allowing it to merge into the cell membrane and pour its contents into the now infected cell. In animal studies, the furin cleavage site appeared to increase the virus’s ability to enter cells. The researchers suspect that the new mutation may further boost entry.
Adrian DENNIS / AFP / Getty Images
The third peak mutation known to be significant is a deletion of six nucleotides in its genetic code, which leads to the loss of two amino acids at positions 69 and 70 in the peak protein. It is not clear exactly what this exclusion does for the virus, but it has appeared several times in different strains, suggesting that it offers an advantage. For now, there is a clear consequence for researchers: exclusion hinders a diagnostic test for SARS-CoV-2. The test is a three-target RT-PCR test, which means it works by detecting three fragments of the SARS-CoV-2 genome, including one in the gene that encodes the peak. When this 69-70 deletion is present, the test will be negative for the spike gene, but positive for the other two SARS-CoV-2 genetic sequences. This result is known as “abandoning the S gene” and is now used to help identify infections caused by B.1.1.7.
These three mutations are the most notable in B.1.1.7 so far. There is little data on the other 20, but researchers are working quickly to try to assess what each can do on its own or in combination with the others.
Severity / mortality from disease
When researchers first raised the concern about B.1.1.7, all of that concern was related to increased transmissibility. Preliminary evidence looking at the results of the infection did not suggest that B.1.1.7 was causing more serious illnesses or more deaths than other strains of the virus. Even so, some saw little comfort in this, as any increase in the total number of infections still leads to more serious cases and deaths in absolute numbers.
The situation became more bleak on January 21, when a UK government advisory group – NERVTAG – found preliminary evidence that “there is a realistic possibility that infection with VOC B.1.1.7 is associated with an increased risk of death compared to infection with non-Virus-VOC. ”
So far, some experts are still not convinced by the preliminary evidence presented and ask for much more data before any conclusions are drawn. On the one hand, the complete data sets behind some of the analyzes done so far have not been published, and some of them relied on comparing small numbers of deaths in people infected with B.1.1.7 with higher numbers of deaths in people infected with other strains. Some experts also wonder whether the calculated increase in deaths could simply be explained by overburdened hospitals, rather than a more deadly variant.
Vaccine effectiveness
With the increase in infectiousness and the possibility of being more deadly, a critical question raised by B.1.1.7 is whether the current vaccines we have – mRNA vaccines from Pfizer / BioNTech and Moderna – will work against the variant. So far, the answer seems to be yes.
On January 19, researchers at Pfizer and BioNTech launched an unrevised peer study, in which they tested blood loaded with antibodies from 16 people who received their mRNA vaccine (BNT162b2) against a pseudovirus that carried the mutated B.1.1 spike protein. 7. The researchers found that vaccine antibodies were as good at neutralizing the pseudovirus with the mutated spike protein from B.1.1.7 as they were at neutralizing a pseudovirus with the spike protein from a SARS-CoV-2 reference virus. “This data … makes it unlikely that the B.1.1.7 strain will escape BNT162b2-mediated protection,” the researchers concluded.
Similarly, on January 25, Moderna launched its own unrevised peer study, which was similar in design. They tested the antibodies of eight people who received their mRNA vaccine against a pseudovirus carrying the mutated B.1.1.7 spike protein. Again, the antibodies neutralized the pseudovirus to levels comparable to those seen with a pseudovirus carrying a reference peak protein.
Yet another similar study, led by researchers at Columbia University and launched on January 26, found the same results. Antibodies from 12 people who received the Modern vaccine and 10 people who received the Pfizer vaccine were able to neutralize a pseudovirus containing the mutated spike protein from B.1.1.7, with only a modest drop in potency compared to neutralization of a pseudovirus carrying a reference spike protein.