The future of cancer treatment may involve personalized vaccines designed to control or even prevent relapses – at least if the new research published on Thursday continues to work. In a small clinical trial, patients with high-risk melanoma who received this vaccine were able to create a long-term, durable immune response to cancer, scientists said. They also remained alive four years after initial treatment, with the majority being actively disease-free.
Cancer vaccines have been a highly sought after goal for scientists for decades. There are two vaccines that can protect against viral diseases that increase the risk of certain types of cancer, HPV and hepatitis B. But developing a widely effective vaccine that can directly prevent the occurrence of cancer has been a more difficult task, thanks to the very nature of the Cancer. On the one hand, cancer cells are mutant versions of the cells found in our body, so our immune system cannot recognize them as enemies as easily as a virus. And since each cancer is specific to each person, it is not so simple to create a vaccine that works for everyone.
In recent years, however, progress has been made in developing cancer vaccines on a more personalized level. The researchers found that tumors carry proteins on the surface of their cells that are not found in normal cells and can make them look different to our immune system. These proteins are called neoantigens. By creating vaccines that train the immune system to better recognize these neoantigens, scientists theorize, we can give our bodies a better chance of fighting a known cancer.
Scientists at the Dana Farber Cancer Institute in Massachusetts and elsewhere have been working on one of these vaccines (called NeoVax) for skin cancer melanoma, as well as glioblastoma, the most common form of brain cancer and very difficult to treat. While your work has showing that the vaccine is well tolerated and appears to create an immune response in patients, only short-term results are available so far. Their new paper, published in Nature Medicine, suggests that his vaccine is also working in the long term.
“These neoantigens are the result of mutations found in a specific tumor – it is created on an individual level. Therefore, our vaccines must be tailored to the patient’s cancer, ”said the study’s author, Patrick Ott, by telephone. “But the news is that, using genomics and sequencing, we can identify these mutations much faster and more cost-effectively than before.”
G / O Media can receive a commission
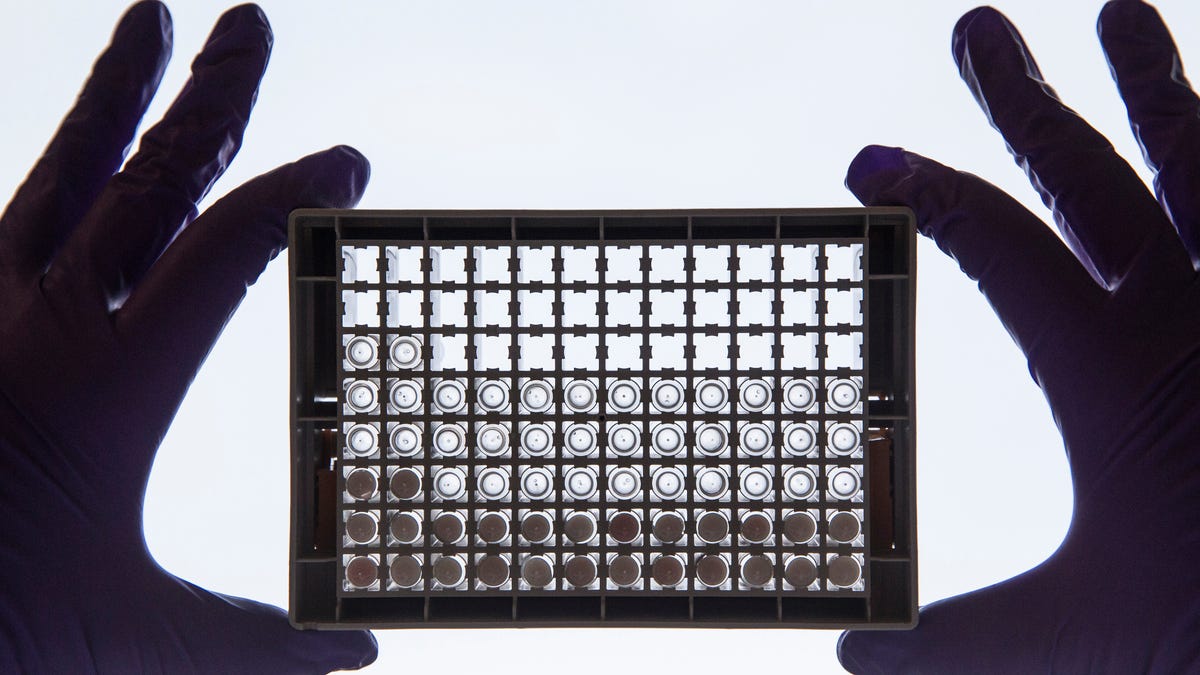
They administered NeoVax to eight patients considered to be at high risk for future, possibly fatal, recurrences of advanced melanoma. They then monitored their health over the next four years, periodically taking blood samples to study the body’s immune response to cancer, in particular tumor-specific T cells.
The vaccine was administered to patients about 18 weeks after surgery to remove the tumor. Ott and his team found that the volunteers continued to load specific T cells for the neoantigens that their vaccine trained the immune system to remember. In some people, they also saw T cells that recognized other neoantigens specific to their tumor. This is an indication that your immune system is adapting to any remaining tumor cells in the body, creating even more weapons against them. All eight patients were still alive after almost four years, with six appearing to be free of the disease at the last check-in.
At the moment, it takes a maximum of three months from a person’s diagnosis for scientists like Ott to create a personalized vaccine. But it is possible that one day these vaccines will be created in a much shorter time, with a simple medical consultation. And while they may not be the “universal” cancer vaccine we all hope for, Ott sees no reason why these vaccines cannot be made to help prevent relapses of any type of cancer.
Vaccines can probably be combined with other treatments. Two patients in the cancer study that spread elsewhere received immune control point inhibitors, drugs that allow the immune system to better target tumor cells. In these patients, the group found evidence that specific tumor T cells found their way into metastatic tumors.
In the future, Ott and his team hope to refine their vaccine technology to create even more potent immune responses that, combined with drugs like immune checkpoint inhibitors, can control cases of advanced cancer. They are also testing their vaccine with other cancers, while continuing to monitor your existing patients.